Chapter 3
Problems of Incidence and Opportunity, 1948-1973
by Henry K. Sharp, Ph.D.
*edited for online viewing, see book for full text
Mason Romaine, a physician with the Virginia State Health Department and director of its new Division of Cancer Control, did not want to panic the commonwealth’s citizens, but he did have alarming news. When Romaine took over the new division dedicated to cancer in 1948, he quickly realized that fatalities due to cancer were having an escalating impact on Virginia’s population and characterized this dramatic acceleration in cancer mortality during the first half of the twentieth century as “appalling.”1 Romaine and other medical practitioners across the nation focused attention on and heightened awareness of cancer research and the resulting development of significant new modalities for treatment, advances reflected in the story of cancer treatment at the University of Virginia.
Practical advances at the University, however, came slowly. Both financial restraints and the actions of individuals would be major factors in the actuality of cancer research and treatment at University Hospital. One early major setback was that Vincent P. Hollander, the highly regarded young internist appointed coordinator of the hospital and medical school cancer programs in December 1952, found that his obligation to the U.S. Air Force compelled him to ask for a multiple-year leave of absence only three months after arriving at UVa. Dean of the medical school, Thomas H. Hunter, presented this event in the best possible terms, but one can easily discern disappointment in his report to the University president: all the new cancer programs were delayed, coordination of the instruction on cancer reverted to faculty members who lacked Hollander’s credentials, and cancer research projects slowed to a virtual standstill without clear leadership.2 Nevertheless, during Hollander’s absence, Hunter continued to coordinate always limited financial resources for the acquisition of both new technology and the professionals trained to use the machines.
It was not just the needs of treating patients, but also those of the medical school that administrators sought to fulfill and which could be used to gain the monies for new materials. For example, Vincent Archer, like Hunter, continued to pressure University administration to provide for cancer-related projects and needs. And by 1960, he had gained another faculty position for radiotherapy to bring the department’s residency training into conformance with new standards the American Board of Radiology promulgated.3
In the mid-1950s, Dean Hunter and others faculty assisted with plans for a major expansion to the medical complex which included a separate X-ray building.4 Not completed until more than a decade later, the major hospital project came to be known as the multi-story wing. As welders secured the steel frame of the new building, another construction crew raised the metal skeleton of four additional floors on top of the three-story cancer laboratory-clinic-ward facility opened in 1952. Rechristened the Mary Stamps Suhling Research Laboratories in 1959, the then seven-story facility included an elevator tower which would eventually serve another seven-story laboratory to be completed during the second phase of construction. Dean Hunter frankly summarized the situation at the completion of the Suhling Labs:
The School’s total research output has increased substantially in recent years, but with the truly explosive expansion nationally in medical research in the past fifteen years we have fallen behind […] One of the chief bottlenecks in the way of expansion of the research effort in the medical school is still laboratory space despite the new cancer research addition, which is to open this month. Until the second phase of our research laboratory addition can be realized, no relief from this pressing problem is in sight.5
Hunter and other physicians nationwide recognized that the way of the future for medicine in general—and for cancer treatment in particular—required an ever-increasing commitment to research activities.
In 1957, as University and state authorities debated designs for the multi-story hospital and enlarged cancer research building, the Soviet Union launched the Sputnik satellite. Cold war competition was in full swing and, as a result, the threat and promise of the atom surged rapidly to the fore of the public imagination. As World War II had previously, the atomic age also energized medical research. A better understanding of radiation promised real medical progress. The substantial funding awarded to UVa radiobiologist William B. Looney by the U.S. Atomic Energy Commission, the American Cancer Society, and the U.S. Public Health Service indicates the therapeutic potential this direction of research held and the array of interests involved. During the 1960s a new phase of medical research commenced, wherein research programs which did not provide immediate results or application at the practical level were not only supported but also encouraged.
The most portentous medical research undertaken during the post-war period—going beyond even that of nuclear medicine—opened the door to what became a highly effective mode of cancer therapy. Chemotherapy, as a concept, originally denoted drug treatment of any disease. It was only with the refinement of the scientific method of experimentation and the development of reliably predictive animal models in the twentieth century that chemical analysis of potential cancer drugs became feasible.6
At UVa, as early as 1959, chief surgeon William “Harry” Muller sought to augment his staff with “individuals who are trained or have an interest in the surgical aspects of metabolic diseases and cancer chemotherapy.”7 Accordingly, the next year he requested that the University appoint two more general surgeons to the staff, “one with interests in cardiovascular or cancer research.”8 It was at this point that inter-specialty competition among physicians in the hospital adversely affected integrative cancer care in what had become a pattern at UVa.
It is important to trace then the management of cancer projects at University Hospital in the 1960s. Internist Vincent Hollander had returned to the directorship of the University’s cancer programs in 1957, and had been named an American Cancer Society Professor of Internal Medicine in 1960. That same year Hollander recruited biochemist Robert M. MacLeod to the cancer research program. Hollander managed funding for cancer training and research projects, including six NIH grants. Yet, despite his success at garnering financial backing for cancer research and education, he faced several difficulties in his position as the new Cancer Coordinator. He was one of the first in an emerging category of physicians, trained specifically in oncology and focused on research not clinical practice. Furthermore, Hollander was not a surgeon and surgery was still considered the primary therapy to treat cancer, along with radiology. He reportedly left the University in 1963 because of a “lack of professional and academic colleagueship” on staff.9
Consequently, in 1964, it was the chief of surgery, Muller, who asked for a surgical staff replacement “in the fields of cancer and clinical cancer coordination”—the position Hollander had held.10 J. Shelton Horsley, a young surgeon from Richmond, Virginia, joined the staff in 1965 as an assistant professor of surgery and the Cancer Coordinator.11 Like those coordinating cancer before Hollander, Horsley was a clinician, not a researcher. Horsley’s interests, therefore, remained centered on surgical work and the clinical cancer programs.12 It appears that competition between the services and a lack of institutional commitment to research obstructed the ability of researchers at UVa to lead the field in developing new treatments, such as chemotherapy.13
Despite the University’s general lethargy to research in cancer programs, there was encouraging news about chemotherapy by the end of the 1960s. After many years of research and clinical trials, medical scientists had proof that chemotherapy could effect “the cure of patients with childhood acute leukemia and … advanced Hodgkin’s disease” in adults.14 Both of these are hematologic, or blood-based cancers, originating in the bone marrow for leukemia and in white blood cells for Hodgkin’s. Previously, hematologic malignancies had been treatable only with radiation. At UVa, the Department of Hematology rose to national prominence during the 1960s as its chair, Byrd S. Leavell, quickly translated these research advances into new treatment options for patients. Indeed, by the end of the decade, the University Hospital was renowned for the treatment of lymphoma and is still recognized as a leading center today. The post-World War II research movement had brought about a new treatment option and a new glimmer of hope in the battle against cancer.
These successes inspired significant changes to cancer programs nationwide and at the University — specifically, the rise of internal medicine relative to surgery and radiology in the field of cancer. As previously discussed, from the first day Paul Barringer opened the hospital doors in 1901, the University had included a medical service, along with surgery, gynecology, and obstetrics. Yet in light of the available cancer therapy options—surgery and radiotherapy—other medical specialties held only a peripheral role in cancer care for many decades. That condition changed demonstrably in 1970, when the medical school and hospital administration established the division of medical oncology, two years before the American Board of Internal Medicine certified medical oncology as an officially recognized subspecialty of the field.15
Within the new field of oncology, much of the initial chemotherapy research had been pursued by hematologists, and the demonstrated victories that had occurred did concern blood-based cancers. Nonetheless, other researchers concurrently developed an interest in applying the same principles to solid tumors, which at least initially lay outside the particular expertise of hematologists. Furthermore, these individuals sought to coordinate cancer research and treatment more globally and in a formally recognized manner.16 As was the case with the University of Virginia, some medical schools and hospitals united the two areas into a single operating division. UVa’s Division of Hematology-Oncology existed as two sub-specialties until they were brought together under the direction of faculty member Peter J. Quesenberry during the 1980 academic year. Even before the fusion of the two fields, Munsey S. Wheby, director of the hematology division, had established several joint teaching and patient care conferences with related disciplines, one of which was with the oncology division shortly after its establishment.17

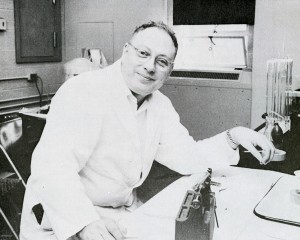
Dr. B. Winfred Ruffner, 1972. University of Virginia Visual History Collection (RG-30/1/10.011). Special Collections, University of Virginia Library.
The task of making a place for medical oncology at the University fell to B. W. Ruffner in 1971, the first head of the new division. Gerald Goldstein joined Ruffner as co-director of the division in 1972. Notably, in addition to offering medical school courses, Ruffner and Goldstein also directed the education of their colleagues. It is through their attempts for further professional education that we have a unique insight into the development of oncology as a field, and of patient care more generally. Specifically, they described the critical role of “[p]roviding emotional support for patients and their families.”18 This was the first official statement in University hospital records on an aspect of cancer care that by the twenty-first century had become an integral part of the therapeutic process. It is important not to underestimate how revolutionary this new concept of patient support was for medical practice in the 1970s. In the absence of official programs, hospital nursing staff had previously provided support services for cancer patients and their families on an informal basis, beginning at least in the 1960s. Agatha van der Erve, an R.N. who joined the radiation oncology unit in 1965, served, in a sense, as a translator and communicated for both patients and medical staff, breaking down the sometimes complex language of physicians for patients and contextualizing the concerns of patients for their physicians.19 Nursing faculty member and medical service supervisor Mary Jane Morris initiated the Reach For Recovery Program at University Hospital in 1968. Later adopted as a national program by the American Cancer Society, Reach For Recovery volunteers provided advice and counseling for women enduring the rigors of breast cancer and the physical and emotional difficulties that surgical treatments sometimes presented for the women and their families. Morris trained nursing staff in cancer care, coordinated volunteers, visited patients and their families, and developed a highly-tuned sense of diplomacy and tact in offering assistance.20
In addition to educating his peers about the value of the nursing model for total patient care, Ruffner also had to build up the division’s clinical service. Over the first two years of operation, the numbers of clinic visits, new patients, and consultations doubled. In 1972, the American Medical Association endorsed “the University of Virginia Hospital as one of 50 places in the country where adequate cancer care can be obtained.”21 Within another year Ruffner could report that physicians from as far away as Florida and California were referring patients to Virginia and that “local patients stay instead of going elsewhere” for “top quality” care.22 Almost immediately upon his appointment, Ruffner began to lobby University authorities to establish a multi-disciplinary cancer clinic “which would make it possible […] to expand and begin new activities such as cancer screening.”23 In such a facility, “patients [could] be seen by surgeons, radiotherapists, and internists at the same time and place, expediting important patient care decisions.”24 Likely without knowing it, Ruffner had reprised the cancer hospital idea that surgeon Edwin Lehman and roentgenologist Vincent Archer had first proposed to the University administration in 1933.
This time, however, the idea of a multi-disciplinary clinic grew out of an important piece of federal legislation enacted in 1971. The National Cancer Act, born of the optimistic spirit that the recent successes in chemotherapy had engendered, aimed to create a broad-reaching national program that would accelerate the pace of cancer research and its translation into treatments and prevention for cancer patients.25 Congress and President Nixon declared war on cancer. The act’s mandates included: establishing several professional advisory panels to develop new national programs and policies; providing the National Cancer Institute (NCI) access to new budget streams; and, most importantly, vesting the NCI with the authority to promote cancer education programs for medical professionals, to initiate new research in its own facilities, to issue grants for research projects elsewhere, and to establish, certify, and fund a national network of cancer centers at universities and research institutions nationwide. These centers, in turn, would adopt “broad-based, coordinated, interdisciplinary programs in cancer research” to translate research more effectively from the laboratory into clinical trials (research studies) and finally into clinical practice.26
The new federal framework for cancer research and treatment was conducive to the goals of cancer specialists at UVa. Ruffner and others, including biochemist and cancer research program director Robert M. MacLeod, pathologist David E. Smith, and radiation oncologist William C. Constable, began the planning process to establish UVa as an NCI-designated cancer center. Federal recognition would have greatly increased the available resources for cancer research. Official designation would have enhanced the University’s reputation and ability to attract superior students, post-graduates, and faculty with particular interests in the cancer question.
In a deflating turn of events, the NCI rejected UVa’s application for cancer center designation in 1973.27 The lost opportunity had immediate repercussions. William Constable directly stated that radiology had no new applicants for its residency program in 1973 because Duke University,
now has funding for a comprehensive cancer center and [is] able to offer the residents more handsome remuneration. Undoubtedly, the absence of a cancer center at the University of Virginia will continue to impede our recruiting of residents who wish a comprehensive training.28
Moreover, the University began to lose some of its prized staff after its failure, including pathologist and the new director of Cancer Studies, David Smith.
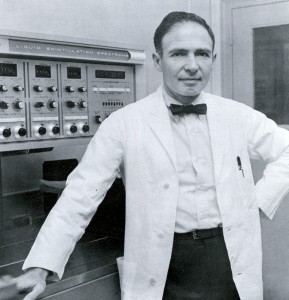
Dr. Robert R. Wagner poses with a liquid scintillation spectrometer, 1968. Historical Collections, HSL, UVa.
On his departure, Smith turned over his files on the cancer center project to Robert R. Wagner, chair of microbiology. It is likely that at this juncture Wagner and others assessed alternatives and developed a new strategy to obtain both organizational support and federal designation. A full decade would pass before the University’s medical administration established a formal cancer center within the medical system, with Wagner leading that initiative.29
The parallel failure of nerve, or of vision, which sank the cancer hospital proposal for the McIntire donation in the 1930s is striking. There, too, University administration chose not to organize and fund a separate cancer facility, opting instead for a weekly clinical meeting to promote collaboration between the specialties. But as in that period, cancer research and care would continue its inexorable development, and the University’s trajectory—at times ahead of the national curve and at other moments behind—itself mirrored the progress and setbacks that many cancer patients themselves come to know over the course of the disease.
- The Virginia Cancer Bulletin 1, no. 1 (1948): 1-3. [↩]
- Tom Hunter, Dean’s Report, 1953 and 1954, Annual Reports to the President, 1904-1958, Accession # RG-2/1/1.381, Special Collections, University of Virginia Library; “Hollander Leaves For Tour Of Duty With Air Force,” The Draw Sheet 1, no. 4 (March 1953): 1. [↩]
- Radiology, 1958-1959, Box 1 and Vincent Archer, Radiology, 1959-60, Box 2, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- “Capital Outlay Requests: University of Virginia Hospital,” UVa Medical Alumni News Letter 7, no. 3 (March-April 1955): 5. [↩]
- Thomas H. Hunter, Dean’s Report, 1959-1960, Box 2, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- Ibid., 8643. [↩]
- William Muller, Surgery, 1959-1960, Box 2, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- William Muller, Surgery, 1960-1961, Box 2, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- This motivation behind Hollander’s departure was recollected by David Smith and communicated to M.C. Wilhelm, 12 August 2008. [↩]
- William Muller, Surgery, 1964-1965, Box 12, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- Surgery, 1965-1966, Box 15, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- Surgery, 1967-1968, Box 19, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- “Dr. Horsley Receives Cancer Society’s Highest Award,” UVa Medical Alumni News Letter 26, no. 1 (November-December 1973): 2. [↩]
- Vincent T. DeVita, Jr., and Edward Chu, “A History of Cancer Chemotherapy,” Cancer Research 68, no. 21 (November 2008): 8648. [↩]
- Gretchen Krueger, “The Formation of the American Society of Clinical Oncology and the Development of a Medical Specialty, 1964-1973,” Perspectives in Biology and Medicine 47, no. 4 (Autumn 2004): 548. [↩]
- Gretchen Krueger and George Canellos, “Where Does Hematology End and Oncology Begin? Questions of Professional Boundaries and Medical Authority,” Journal of Clinical Oncology 24, no. 16 (June 2006): 2584; DeVita, 8650; and Krueger, “Formation,” 549. [↩]
- Munsey Wheby, Internal Medicine, Division of Hematology, 1970-1971, Box 29 and Internal Medicine, Division of Hematology, 1971-1972, Box 31, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- B. W. Ruffner, Internal Medicine, Division of Oncology, 1971-1972, Box 31, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- Agatha van der Erve, interview by M.C. Wilhelm, video recording, 5 February 2009, UVa History of Cancer Care Project, Charlottesville, Va. [↩]
- Mary Jane Morris, interview by M.C. Wilhelm, video recording, 28 January 2009, UVa History of Cancer Care Project, Charlottesville, Va. [↩]
- B. W. Ruffner, Internal Medicine, Division of Oncology, 1971-1972, Box 31, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- B. W. Ruffner, Internal Medicine, Division of Oncology, 1972-1973, Box 33, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- B. W. Ruffner, Internal Medicine, Division of Oncology, 1971-1972, Box 31, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- B. W. Ruffner, Internal Medicine, Division of Oncology, 1972-1973, Box 33, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- National Cancer Institute, “The 1971 National Cancer Act,” http://legislative.cancer.gov/history/phsa/1971, accessed on 13 November 2010. [↩]
- National Cancer Institute, “The National Cancer Institute Cancer Centers Program,” http://ncccp.cancer.gov/About/ProgramSummary.html, accessed on 13 November 2010. [↩]
- David Smith conversation with M.C. Wilhelm, 12 August 2008. [↩]
- William Constable, Division of Radiation Oncology, 1972-1973, Box 34, Annual Reports to the President, 1958-1974, Accession # RG-2/1/1.841, Special Collections, University of Virginia Library. [↩]
- David Smith, conversation with M.C. Wilhelm, 12 August 2008; Cancer Studies Division, Box 15:11, The Papers of Dr. Edward Watson Hook, Jr., 1947-1998, CMHSL; “Wagner Named Head of Cancer Center,” Helix 2, no. 2 (Spring 1984): 20; Memorandum of Gary Holdren and Jane Ikenberry Dorrier to Members, Hospital Long Range Planning Committee, 10 September 1984, Box 60:4, HEDO, CMHSL. [↩]