Introduction
A Legacy of Care: Cancer and Thomas Jefferson
by Victoria N. Meyer, Ph.D.
*edited for online viewing, see book for full text
Jefferson Portrait by Gilbert Stuart, 1805. Image courtesy of the National Portrait Gallery, Smithsonian Institution and the Thomas Jefferson Foundation.
After a decade of estrangement, former presidents Thomas Jefferson and John Adams were enjoying their recently renewed friendship in the summer of 1813 when tragedy struck. Adams wrote Jefferson that his only daughter Abigail “Nabby” Smith had died from breast cancer at the age of forty-nine.1 Abigail Adams revealed the hope that the family had after Nabby had survived the excruciating removal of her left breast two years earlier. Abigail wrote, “we flatterd ourselves that the cure was effectual, but it proved otherwise. It soon communicated itself through the whole mass of the Blood, and after severe sufferings, terminated her existance.”2
Less than two months before her death, Nabby had returned to the home of her parents where she was cared for, above all, by her attentive father.3 As to the torment of her family, who weathered with Nabby the devastation that cancer wreaked, Jefferson commiserated saying, “I know the depth of the affliction [your loss] has caused, and can sympathise with it the more sensibly, inasmuch as there is no degree of affliction, produced by the loss of those dear to us, which experience has not taught me to estimate. I have ever found time and silence the only medicine, and these but assuage, they never can suppress…”4
The reality of Nabby’s illness was years of pain for her, worry for her family, and despair for all at the limited treatment options available. Even Jefferson, who generally avoided physicians when he could, would have recommended consulting a doctor in a case of suspected cancer.5 At first, Nabby’s physicians suggested medicines to purge her cancer, but the famed physician and founding father Benjamin Rush wrote to her parents in June 1811 with disheartening news. Although he did not eliminate the possibility of recovery, he had concluded from her own descriptions of her now misshapen breast that the only “remedy [was] the knife” and cautioned that “there be no delay in flying to the knife.”6 Nonetheless, Rush recognized that the invasive surgery to remove the cancerous tumor would be a difficult and terrifying decision to accept.

Instruments for breast surgery, Goussier, Louis-Jacques, Livourne : L’impreimerie de éditeurs, 17–. Image courtesy of National Library of Medicine.
Despite the torment of her surgery, the outlook for Nabby’s recovery appeared promising. Rush even congratulated John Adams, assuring him that “her cure will be radical and durable. I consider her as rescued from a premature grave.”7 Her family and physicians believed that surgery had offered her the one hope of a cure. Contemporaries most often did not understand a successful treatment or ‘cure’ for cancer to mean permanent elimination of the disease but merely additional time. This bleak outlook is perhaps why cancer was one circumstance in which Jefferson argued the acceptability of ending one’s life as “the rational relief.”8 The Adams’ optimism that her cancer was completely eliminated was atypical and led to crashing disappointment when it reoccurred.
Physicians worried about the growing phobia of cancer. Benjamin Rush warned, “To pronounce a disease incurable, is often to render it so.”9 How to deconstruct cancer as an untreatable disease would be one challenge faced by health professionals in the coming centuries. This illness—cancer—was not something openly discussed outside of the private sphere in the nineteenth century, despite the widespread misery it generated. Indeed, perceptions and reactions to the malady played a significant role in the medical approach to cancer throughout its long history from the time the Greeks recognized cancer as a distinct disease and coined the term karkinoma, Greek for ‘crab’.
Beneath the conceptual unity of the term ‘cancer’, there were various understandings and treatments of the disease in its diverse forms. Yet, reliable treatments or cures proved elusive. This was true for breast cancer, the base of all early studies of cancer. Hippocrates specifically mentioned cancer of the breast and both Leonides and Galen described the surgical removal of the breast.10 Despite these surgical efforts since antiquity, successful treatment of breast cancer did not significantly elevate one’s long-term chances of survival in comparison to other forms of the disease, nor did it improve through the centuries.
In light of the well-known incidence of cancer during the nineteenth century, Nabby Smith and the Adamses were likely not the only members of Thomas Jefferson’s circle decimated by the illness. Although cancer was not a particular focus of Jefferson’s studies, the incidence and treatment of cancer correlated to the former president’s lifelong interest in matters of health and medicine. Jefferson’s disdain for many of the contemporary medical practices has been well-documented.11 He argued that physicians were inexperienced in practice and relied upon unfounded theories and trickery. As a result, Jefferson charged each person to maintain his or her own health and to resort to an enlightened physician only when absolutely necessary.12 Jefferson recognized, however, that his contemporaries faced a dilemma: how to care for their own bodies or to find an enlightened physician, when medicine was so corrupted?

Robley Dunglison, first medical professor at UVa and Jefferson’s personal physician. Historical Collections, HSL, UVa.
Jefferson found a novel solution to this predicament a few years after Nabby’s death when he developed a new type of institution for higher education. In 1819, Jefferson began designing a university to be located in Charlottesville. At the University of Virginia, which would open for classes in 1825, students would receive a broad education. Medical studies would be a foundation of academics, intended not just for those who would pursue a career in medicine but for all students. Graduates would leave as well-informed guardians of their bodies and those from the medical school would have been rigorously trained as enlightened doctors. Regarding the inexperience of physicians and theoretical emphasis of medicine, Jefferson asserted, “It is in this part of medicine that I wish to see a reform, an abandonment of hypothesis for sober facts, the first degree of value set on clinical observation, and the lowest on visionary theories,” a medicine based on “observation and experiment.”13 To this end, Jefferson hired Robley Dunglison to teach anatomy, surgery, history of the progress and theories of medicine, physiology, pathology, materia medica, and pharmacy.14 Dunglison became the first state-supported, full-time clinical professor in a university medical school in the United States. Jefferson envisioned that a new generation of rigorously-trained physicians would emerge from UVa and help strengthen the health, and thus society, of America.
The private world of cancer diagnosis and treatment was irrevocably shattered in 1884, just years before we begin our exploration of cancer care at the University of Virginia. The origins of the modern, public dialogue between laymen and medical practitioners about cancer can be traced to the medical ordeal of another former U.S. president. In late spring of 1884, General Ulysses S. Grant began to experience pain and discomfort in his throat.15 Like many of his contemporaries, Grant delayed seeking medical treatment despite his suspicion that something was wrong. Even after Grant’s initial visit with a doctor, he postponed following up with his own physician for three months.16
A culture of silence surrounding cancer resulting in the patient and family suffering in isolation fractured in the 1880s as a result of Grant’s illness. Once he had finally seen his personal physician, Grant was immediately referred to a throat specialist, John H. Douglas, who concluded that Grant had throat cancer. Aware of the powerful effect of the word ‘cancer’ on patients, Douglas reportedly only told Grant that “his throat was affected by a complaint with a cancerous tendency.”17 Grant’s reluctance to seek medical care had allowed the cancer to flourish unchecked and eliminated surgery and any other remedies. His sqaumous-cell carcinoma had spread from the tonsil to the mouth, neck, and soft palate.18 Radical surgery—which would have removed large portions of his soft palate, all of his tongue, and much of his lower jaw—was considered, but then quickly dismissed.19
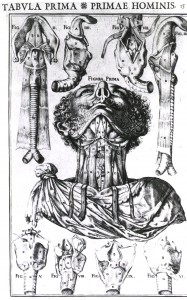
Anatomical view of the throat in nine illustrations. Casserio, Giulio, De vocis auditusque organis historia anatomica singulari fide methodo, tabula prima, pl. 15. Image courtesy of National Library of Medicine.
As has happened often in recent decades, the diagnosis of a beloved celebrity with a lingering painful disease captivated public attention. While normally the word ‘cancer’ did not even appear in popular newspapers, by March reporters had seized upon Grant’s illness and they wrote numerous stories until his death in July of 1885.20 The articles emphasized the sensational aspects and inherent drama of the former president’s painful demise, turning his illness into a sideshow. As a result of the print explosion, Grant’s illness paved the way for both popular and medical discussions of cancer in the public sphere by the last decade of the nineteenth century, altering perceptions and treatments of disease in the century to come.
The twentieth century, the focus of this book, would come to be a time of revolution in not only popular discussion and understanding of cancer, but also in the medical ability to diagnose and treat the disease. The word ‘cancer’ still has an undeniable hold on the fears of modern Americans, but in the last decades patients have reasserted control over their bodies. This became possible through the collaboration of medical practitioners, patients, and government officials who continue to emphasize preventative action against cancer: public awareness of the illness, routine screenings, and early diagnosis. And, although Jefferson had not originally envisioned a hospital at the University of Virginia, the demands of a heavily populated, industrial, and modernizing society necessitated the establishment of an institution to offer advanced care to all citizens. The unique demands of cancer, both social and medical, also compelled the medical system and public to adapt in the twentieth century. As a result the narrative of cancer in the United States, and the unique role of the University of Virginia, is the story of setbacks and innovations. One in which the definition of ‘success’, like ‘cure’, is ever-changing.
- John Adams to Thomas Jefferson, Quincy, MA, 16 August 1813, in The Adams-Jefferson Letters: The Complete Correspondence Between Thomas Jefferson and Abigail and John Adams, ed. Lester J. Cappon (Chapel Hill: The University of North Carolina Press, 1959), 2:366. [↩]
- Abigail Adams to Thomas Jefferson, Quincy, MA, 20 September 1813, in The Adams-Jefferson Letters, 2:377. [↩]
- James S. Olson, Bathsheba’s Breast: Women, Cancer, and History (Baltimore: The Johns Hopkins University Press, 2002), 43. [↩]
- Thomas Jefferson to John Adams, Monticello, 12 October 1813, in The Adams-Jefferson Letters, 2:386. [↩]
- Jock Murray, “Thomas Jefferson and Medicine” Journal of Medical Biography 5 (August 1997): 149. [↩]
- Benjamin Rush, Letters, ed. L.H. Butterfield (Princeton, NJ: Princeton University Press for the American Philosophical Society, 1951), 2:1104. [↩]
- Olson, 42. [↩]
- Murray, 155. [↩]
- Benjamin Rush, “An Account of the Late Dr. Hugh Martin’s Cancer Powder, with Brief Observations on Cancers” Transactions of the American Philosophical Society 2 (1786): 216. [↩]
- Hippocrates mentioned it in his Epidemics I and VII as well as his Diseases of Women. Galen specifically addressed cancer in his De tumoribus praeter naturam. [↩]
- See, for example, S.X. Radbill, “Thomas Jefferson and the Doctors,” Transactions and Studies of the College of Physicians of Philadelphia, 4 ser., 37 (1969): 106-14; C.R. Hall, “Jefferson on the Medical Theory and Practice of his Day,” Bulletin of the History of Medicine 31 (1957): 235-45. [↩]
- Louis S. Greenbaum, “Thomas Jefferson, the Paris Hospitals, and the University of Virginia,” in “Thomas Jefferson, 1743-1993: An Anniversary Collection”, special issue, Eighteenth-Century Studies 26, no. 4 (Summer 1993): 621-22. [↩]
- Thomas Jefferson, The Jeffersonian Cyclopedia: A Comprehensive Collection of the Views of Thomas Jefferson …, ed. John P. Foley (New York: Funk & Wagnalls Company, 1900), 547 and 905. [↩]
- Greenbaum, 624. [↩]
- Andrew Renehan and John C. Lowry, “The Oral Tumors of Two American Presidents: What If They Were Alive Today?” Journal of the Royal Society of Medicine 88 (July 1995): 377. [↩]
- Ibid. [↩]
- Thomas A. Sebeok, “Grant’s Final Interpretant” MLN 100, no. 5 (December 1985): 922-923. [↩]
- Renehan and Lowry, 378. [↩]
- Ibid. [↩]
- James T. Patterson, The Dread Disease: Cancer and Modern American Culture (Cambridge, Mass.: Harvard University Press, 1987), 3 and 10-11. [↩]