Physician Fee Bills by Todd L. Savitt, Ph.D.
Medicine is a calling – a profession. Practitioners pledge to care for ailing people in their time of need, a time when they are most vulnerable. As noble as the profession of medicine is in fulfilling this goal, those who practice it are also earning a living. Thus one cannot discount the business aspect of medical practice. A physician, no matter how skillful and loved by his patients, must earn a sufficient amount of money and goods to live a life. Documents exist that provide insight into this fiscal aspect of the medical profession. One can find letters to and from patients, bills and receipts, occasional medical journal articles and books, and other evidence. A most interesting kind of evidence documenting the business side of medicine is the Fee Bill.
Fee Bills provide a large amount of information about medical practice and the medical profession. In the late 18th, throughout the 19th, and on into the early years of the 20th centuries, fee bills in the United States served several purposes. First, however, here is some background information about medicine and medical practice at the time of the Charlottesville Fee Bill:
For the most part, physicians during these years practiced solo, and, in areas where there was an abundance of medical practitioners, competed with one another for patients. As the number of medical schools grew during the 19th century, so did the number of physicians in practice. Many small towns and hamlets in the country could boast of at least one physician. The radius of a physician’s practice was limited by the distance he or she (mostly he) could reasonably travel to make house calls. (Most patient-physician interactions occurred in the patient’s home rather than at the physician’s office throughout the 19th century.) These “service areas” often overlapped with the service areas of other physicians and thus allowed for competition among physicians for patients. One way that physicians gained an edge over competitors in the quest for patients was to charge less than their fellow healers.

Patent medicine label for unnamed women's hair tonic which "restores gray hair ... cures dandruff, and prevents baldness," printed between 1830 and 1870. Courtesy of Library of Congress Prints and Photographs Division, Washington, D.C., accessed 30 August 2011.
Another source of medical practitioner competition was the presence of non-regularly trained healers – so called “irregular practitioners.” Among the “irregulars” were Thomsonians (followers of Samuel Thomson, who used botanic remedies rather than the metallic medicines of the regulars), Homeopaths (followers of Samuel Hahnemann, who believed that highly diluted solutions of medicine were more effective than more concentrated preparations, and that a medicine that produced a certain symptom cured that symptom [like cures like]), and Hydropaths (who believed that the use of pure water, inside and outside of the body prevented and cured disease).
To combat these irregular healers and those regularly trained physicians who charged low fees, physicians in a town, city, county, or region joined together. Sometimes they organized formal medical societies where physicians could meet and exchange information about medical treatments, get suggestions on ways to treat difficult cases, develop collegial relationships for times when consults on difficult cases were needed, attempt to regulate who could practice medicine in their area, and, most significant for our purposes, establish a standard set of fees for treatments and procedures. Sometimes physicians did not found associations, but simply met and agreed to a set of fees that all would adhere to. Those agreed-upon charges-for-service, known as fee bills, were usually printed and posted or circulated or published in newspapers.
As might be expected, there was some pressure on all “respectable” physicians in an area to join the others in establishing a fee bill, but, as also might be expected, some healers refused to be restricted by a fee bill and charged what they wished, often undercutting those who belonged to the group. Naming the physicians who signed the fee bill served to advertise to the population who among local healers were the trained, respectable physicians and who were the low-cost (and, according to the regulars, presumably less competent) healers – the irregulars and quacks. Patients were thus “protected” from unscrupulous practitioners. In areas where physicians did not develop fee bills, patients could also be over-charged by these unscrupulous practitioners.
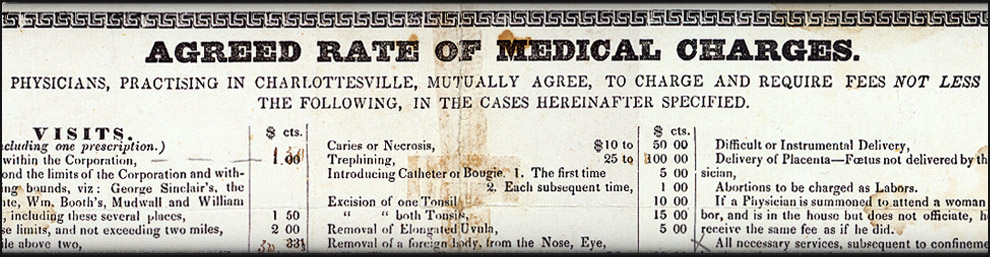
Some fee bills, like the 1848 Charlottesville document, were quite detailed. Others were less specific and provided only fee ranges and general categories of healing activities. The more detailed the fee bill, the more interesting and instructive it is to present-day readers.More than thirty years before the Charlottesville doctors signed their fee bill, a similar one was printed in a Fredericksburg, Virginia, newspaper, as seen to the right. It informed the public that the scale of charges, either a set fee or a range depending on the service, would “promote harmony and justice” among the doctors and protect “the Profession, as far as practicable, from all competition except that founded on merit.” Among the things one can learn by studying a medical fee bill are:
- What treatments physicians used and procedures physicians performed during a certain time period. Though we may smile at some of these medical interventions, safe in our 21st century medical world, those treatments and procedures were the accepted medicine of the day and taken very seriously by practitioner and patient alike. Remember: Folks a century from now may smile at some of the medical treatments we use today.
- The state of the society in which physicians practiced, as, for example, when black slaves are mentioned because fees for their care differed from that of white folks.
- The value physicians and patients placed on medical care. One can also learn how the value of currency has changed over time.
- The economic forces existing in a region by the payment arrangements spelled out in some fee bills, both in terms of the time and frequency of expected payments, and the mode of payment.
Let’s look in detail at the Charlottesville Fee Bill and see what we can learn, section by section:
Title:
The twelve physicians who promulgated this fee bill did not identify the document by that name. Instead, they gave it a title that made clear their intentions: They wanted non-signator local physicians and medical practitioners as well as the literate general public to know that a group of regular doctors had banded together to protect their own and the public’s interest by publishing the minimum fees they would charge for medical care. They provide no explanation of their perceived need for such a document. Had the regular physicians in Charlottesville been incurring strong competition from other practitioners in the weeks and months before June 9, 1848? Had some regular physicians been charging very high fees that upset local residents? Or very low fees that upset other regulars?
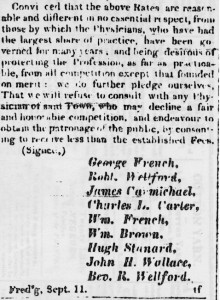
Saddle bag for carrying medicine on horseback, c. 1800s. Historical Collections, The Claude Moore Health Sciences Library, University of Virginia.
Visits:
Most of us think of the antebellum South as a place where life moved along at a rather unhurried pace, except perhaps at planting and harvest times when agricultural workers, enslaved and free, labored under weather threats. For physicians of that period practicing in rural areas like Charlottesville and Albemarle County, time was money, just as it is today. Physicians saw most of their patients in the sick person’s home, so they were on their horses or in their buggies many hours a day. Travel to a distant farm, plantation, or home meant less time to see other patients. And less income. So time issues appear on fee bills. The Charlottesville Twelve, like doctors around the country, took travel time into account in figuring patient charges. They established one fee for seeing patients within Charlottesville’s corporate limits, another for visits outside of town but within an area bounded by well-known citizens’ land, a third for trips within two miles beyond these named bounds, and then a set mileage fee for journeys beyond that. They also included an inconvenience factor in their fee schedule, specifying charges for trips at night, in inclement weather, and for frequent visits to the same patient (in the last situation by not allowing lower fees per visit).
Consultations:
Sometimes physicians find that cases are beyond their knowledge, experience, or skills and require additional expertise. Doctors nowadays refer patients to specialists whom they know and trust, and then receive a report back from the consultant about the diagnosis and the treatment provided or recommended. The referring physician, unless he or she has an arrangement with a specialist to be paid a portion of fees collected as a reward for sending patients to that specialist (which is illegal and unethical), receives no financial compensation.
In the 19th century, when a physician requested a second physician’s opinion on a patient’s case, both physicians together customarily visited the patient at the bedside. They then discussed the findings and reported them to the patient and/or the patient’s family. As this Charlottesville Fee Bill indicates, both physicians expected payment for their time and expertise, not just the consulting practitioner. (Occasionally, 19th century physicians were accused of over-using consultants or of having reciprocal arrangements with fellow physicians to use each other as consultants, even when the situation did not warrant it. Patient beware!)
Prescriptions:
In a rural practice, patients expected that physicians would provide the medications required for treatment. Pharmacies existed in towns and could provide farm and plantation dwellers with supplies of commonly used home remedies or ingredients to prepare a home remedy. But when a physician prescribed a special medication not usually found in a home medicine chest, he compounded it on the spot and charged a fee for it and refills as needed.
Amputations, Operations, Fractures, and Dislocations:
The extensive list of procedures in the Charlottesville Fee Bill provides us with an idea of the procedures practitioners of medicine in mid-19th century America advertised they could perform. Note that most of these procedures dealt with problems on the body’s surface or just beneath it. Even “Excision of Tumor” and “Excision of Cancer” on the Fee Bill meant surface or subcutaneous growths. No procedure listed involved entering the abdominal or thoracic (chest) cavity to perform such now common procedures as appendectomy, hysterectomy, gall bladder removal, or any kind of cardiac surgery. Ether anesthesia had just been introduced into medicine less than two years previously and chloroform just a year earlier, so painless surgery was not widely available in mid-1848. The idea of performing surgery in a sterile environment, free of germs, was still many years away, as it wasn’t until the mid-1870s that the idea of bacteria as a cause of surgical infection and of many diseases was introduced.
One of the commonest treatments that both physicians and laypeople used in the care of many (perhaps most) non-surgical conditions was bloodletting – the intentional removal of a pint and often more of blood from a patient’s body. All three methods of bloodletting are listed under “Operations.” One could use a thumb or spring lancet to cut into a vein, usually at the inside bend of the elbow, where blood for tests or for donation is removed in present days. The person performing this venesection would catch the blood in some kind of bleeding bowl.
Cupping usually involved the use of a spring-loaded multi-bladed instrument called a scarifier or scarificator that made multiple small incisions in the skin over which a glass cup, heated (note the tow in the picture to the right which would have been ignited in the cup) to evacuate available air and create a vacuum, was placed. Blood would collect in the cup, which stuck to the skin until removed by the operator. Some preferred their bloodletting via blood-sucking leeches, which were placed on the skin and allowed to remove the prescribed amount of liquid and then removed.
When looking over the list of procedures on the fee bill, consider the concept of the emergency. Farm accidents, burns from household cooking and heating fires, children’s falls while playing, and any number of other medical situations where quick and decisive action is needed made most rural dwellers in 19th-century America much more medically self-reliant than most of us 21st-century folks are. They had no telephone to contact a poison control center or a 911-medic who could talk them through a medical situation. They could not call for an ambulance or a physician to pick them up or see them on site. They had no automobile to whisk them to a physician’s office or hospital emergency room. Horseback or horse-and-buggy might get you to the doctor’s office, but if he is out visiting other patients, you might not be able to contact him for hours. Rural folks learned to do bloodletting and to improvise in caring for injuries and diseases until they ran out of options and were forced to call the physician. So patients and their families did some of the procedures listed on the Charlottesville Fee Bill for themselves, on themselves.
Obstetrics:
Mid-19th century physicians felt themselves in competition with midwives when it came to delivering children. Until the late 18th century, obstetrics was primarily the domain of women – especially experienced women known as midwives. When the speculum and the forceps were introduced into medicine, physicians began to let it be known that they were better trained to officiate at births than these untrained midwives. This competition is reflected in the Charlottesville Fee Bill in the item stating: “If a Physician is summoned to attend a woman in Labor, and is in the house but does not officiate [i.e., a midwife is in charge of the birth], he shall receive the same fee as if he did.”
The only place in this schedule of charges from physicians practicing in the plantation South where slavery is mentioned is in regard to the birthing of slave children. In all regards but this one, the charge for medical care of enslaved patients was, presumably, the same as for free patients. It is not clear why delivering a black woman was less expensive than delivering a white woman. One possibility is that slaveowners would not pay the same price for black deliveries because they considered blacks lesser human beings compared to whites and thus not of equal value. Certainly in a slave society such as existed in central Virginia, slaves were valuable commodities. But perhaps they were not considered as valuable as white mothers and children.
Attendance:
Again, time was a vital aspect of a rural physician’s economic calculation. Sitting with a patient for more than two hours meant he was not able to see other patients and thus not able to earn more money. So he put a monetary value on his time and charged that amount to his patients. Sometimes the physician would have to sit awake with the patient through the night, thereby losing sleep as well as time. For that service Charlottesville (and other) physicians felt justified in charging an extra fee.
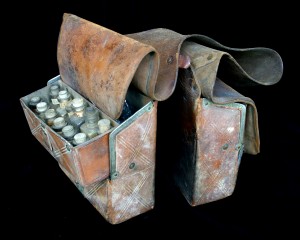
The Final Note:
The last item under “Notes” provides some insight into the financial situation of physicians at this time. Physicians delivered annual bills to their patients at the end of the year, in December, and expected to be paid by the start of the next year, on January 1. Though some patients settled their bills during the year as funds (or bartered goods or labor) came available, most waited until after the harvest when they had collected their crop money to pay the physician. Note the Fredericksburg newspaper advertisement to the right that states the subscribers (Drs. Carmichael and Browne) with the passing of another year “are determined to adhere to their resolution of settling their accounts annually.”
Fee bills can provide some insight into more than what medical procedures were done in a certain time period. They tell us also about aspects of the practice and medicine and the society in which that practice existed.